GENERAL CHARACTERISTICS OF THE CLASS SPOROVITA.
Lesson 3
Class Sporozoa- Sporozoans (Sporozoa)
CLASS SPOROVICS (SPOROZOA)
Type: Protozoa
Class: Sporozoa (Sporozoa)
Order: Bloodspores (Haemosporidia)
Species: Disease:
Plasmodium vivax Three day malaria
Plasmodium malaria
Plasmodium ovale Three day malaria
Plasmodium falciparum Tropical malaria
Subtype Coccidia
toxoplasmosis toxoplasmosis
GENERAL CHARACTERISTICS OF THE CLASS SPOROVITA.
As a result of gametogony, individuals of the sexual generation are formed - gamonts (macrogametocytes and microgametocytes), giving rise to gametes, due to which the sexual process is carried out - copulation. This process occurs in the body of the final host.
Sporogony is the process of division of the zygote, resulting in the formation of worm-like, mononuclear cells - sporozoites, through which the intermediate host is infected.
In all sporozoans, the so-called zygotic reduction is observed: the first division of the zygote nucleus during sporogony is meiotic and all subsequent stages, except for the zygote, are characterized by a haploid set of chromosomes.
Toxoplasma and malarial Plasmodium are of the greatest medical importance due to their pathogenicity and geographic distribution.
Sporozoans (Sporozoa)
In sporozoans, during the sexual cycle of reproduction, when the male and female gametes merge, a spore (cyst) is formed, in which sporozoites are formed. The sporozoites are then transmitted in various ways from one host to another.
Type: sporozoans
Class: Sporozoa
Order: blood spores (Haemosporidia)
Genus: Plasmodium
Style: Pl. vivax
Style: Pl. malariae
Style: Pl. ovale
Style: Pl. falciparum
Medical Significance:
Pl.vivax - the causative agent of 3-day malaria
Pl.malariae - the causative agent of 4-day malaria
Pl.ovale - the causative agent of ovalemalaria (3 days)
· Pl.falciparum - the causative agent of tropical malaria.
It is an anthroponotic natural focal transmissible disease.
The method of infection is mainly through the bite of a female chamber of the genus Anopheles (99.8%), and infection through blood transfusion and transplacental infection is also possible.
The life cycle of Plasmodium occurs with a change of hosts. Plasmodium goes through two stages of development:
Schizogony - asexual stage - in the human body.
Sporogony - the sexual stage - in the body of a mosquito of the genus Anopheles, is an invasive form.
Hosts:
The final host is a female malarial mosquito of the genus Anopheles
· Intermediate host: human.
Malarial Plasmodium. Piasmodium vivax - the causative agent of three-day malaria; Plasmodium malariae - the causative agent of four-day malaria; Plasmodium falciparum is the causative agent of tropical malaria and Plasmodium ovale is the causative agent of three-day malaria (oval).
Life cycle. Malarial plasmodia go through two stages of development - asexual (schizogony) in the human body and sexual (sporogony) in the body of the carrier - female malarial mosquitoes of the genus Anopheles.
Development cycle Plasmodium vivax. Stages of schizogony in the human body (below): 1 - sporozoite; 2-5 - schizogony in the liver parenchyma; 6-9 - schizogony in erythrocytes; 10.11 - gamonts. Stages of sporogony in the body of the Anopheles mosquito: 12 - microgamont; 13 - microgametogenesis; 14 - fertilization; 15 - ookinete (migratory zygote); 16-18 - development of sporozoites; 19 - penetration of sporozoites into the salivary glands of the mosquito (according to Grell).
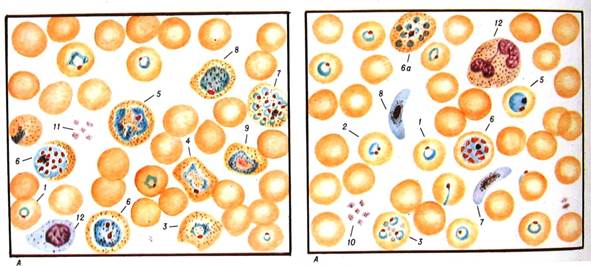
Blood forms of Plasmodium vivax: a - in a smear
1 - annular trophozoite; 2 - deformed annular trophozoite; 3 - young trophozoite; 4 - semi-adult trophozoite; 5 - adult trophozoite; 6 - immature schizont; 6a - mature schizont; 7 - mature schizont; 8 - female gametocyte; 9 - male gametocyte; 10 - reticulocyte; 11 - platelets; 12 - lymphocyte.
With the onset of erythrocyte schizogony, the development of P. falciparum and R. malariae in the liver stops. However, in P. vivax and P. ovale, some of the sporozoites remain in the liver (“dormant”) and, when activated, they cause distant recessives of the disease.
Merozoites that have penetrated into erythrocytes turn into trophozoites (growing forms of an annular or amoeboid form), and the latter into schizonts (dividing forms). Schizonts in the process of division give rise to a new generation of merozoites, which, in turn, penetrate into other erythrocytes. The indicated developmental cycle in erythrocytes is 72 hours for P. malariae or 48 hours for other species.
Some erythrocytes develop male and female sexual forms - gamonts. They complete their development only after entering the body of a mosquito with blood within 7-45 days, depending on the ambient temperature. As a result, sporozoites accumulate in the salivary glands of the malarial mosquito, and such a mosquito becomes capable of infecting humans again.
Clinical picture. Plasmodium malaria causes a serious disease in humans - malaria. The incubation period, depending on the type of malaria, is 8-25 days, with three-day malaria it can reach 8-14 months. For malaria, fever attacks are typical, which are observed at the time of the release of merozoites from destroyed erythrocytes. The onset of the disease is acute, in the morning or afternoon the body temperature rises rapidly, accompanied by chills. After a few hours, the body temperature drops rapidly, often to 35-36°C with the appearance of profuse sweating and weakness.
Tropical malaria is the most severe (body temperature can stay high for several days).
Complications are more often observed in tropical malaria. This is a malarial coma, rapidly progressing and leading to death without urgent treatment, and hemoglobin-uric fever. The latter occurs in individuals with an increased tendency of red blood cells to hemolysis, as a result of a genetically congenital deficiency of the enzyme glucose-6-phosphate dehydrogenase. After taking certain antimalarial drugs (quinine, primaquine, etc.), the patient's body temperature rises, pains appear in the liver, spleen, and lower back. Urine acquires the color of black coffee, contains hemoglobin, protein. Hemolytic jaundice develops. Lethality reaches 30%.
Malaria affects people of all ages, including infants, in whom the clinical picture may differ significantly from the typical. Possible carrier.
The duration of the course of the disease, including relapses and carriage, is 2-3 years for three-day malaria, 6-12 months for tropical malaria, and 2-4 years for oval malaria.
With four-day malaria, patients usually recover within 2-3 years, but carriage in some cases can last up to 50 years. Relapses of four-day malaria after trauma or surgery 10–20 years after the primary disease have been described.
When infected through the blood of a donor, the disease manifests itself after 6-25 days. Vaccinated four-day malaria can occur atypically, manifesting itself several weeks or even months after infection.
Not everyone gets malaria.
sickle cell anemia
· Babies who do not have a / g of the Dafi system.
The greatest danger to the conditions of Russia is R. vivax. This malaria pathogen is characterized by the widest global range and the lowest temperature threshold of development. Almost all species of malarial mosquitoes of the genus Anopheles are susceptible to it, including those characteristic of the fauna of Russia. It has polymorphism on the basis of the duration of exoerythrocyte schizogony, which is explained by the presence of two types of sporozoites: tachysporozoites, which give a short incubation (6-8 days) and bradysporozoites, which give a long incubation (up to 6-14 months). Thus, adaptation to the pathogen's experience of the cold period of the year is achieved, when its transmission by mosquitoes is possible.
Tropical malaria caused by R. falciparum is characterized by the most severe course, a large number of complications and the greatest mortality. Despite its smaller range compared to P. vivax and P. malaria, P. falciparum causes 50% of the world's malaria incidence and 98% of all deaths. A severe form of tropical malaria is the development of malarial coma, accompanied by loss of consciousness and impaired reflex activity of the body. Coma appears to be caused by blockage of brain capillaries by infected red blood cells. In these areas, degeneration of the brain tissue is observed. Coma, as a rule, leads to the death of the patient. It has been established that infected erythrocytes adhere to endothelial cells through membrane outgrowths - "knobs" induced by plasmodia and tightly clog the vessels. Blockage of cerebral vessels contributes to rosetting - the adhesion of healthy red blood cells to infected ones.
The fourth causative agent of human malaria, P. ovale, was found in Russia only in the form of imported cases from the countries of Equatorial Africa and Oceania.
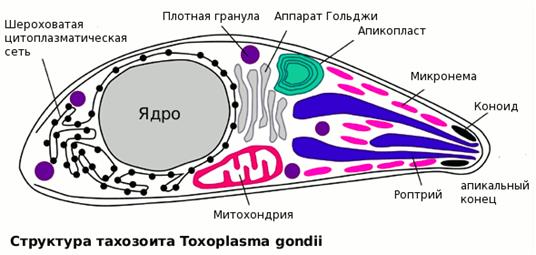
Life cycle. Toxoplasma infects many wild and domestic animals and birds, as well as humans, in whose bodies an asexual cycle of development and reproduction (intermediate hosts) passes.
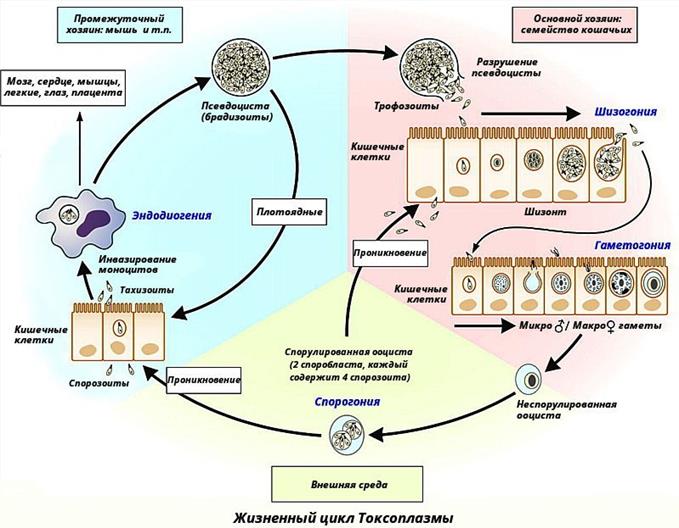
The sexual cycle of reproduction occurs in the cells of the intestinal mucosa of cats (the main host). With the faeces of cats, oocysts are excreted, round, with a dense, colorless two-layer membrane, 9-14 microns in diameter. Oocysts mature and are well preserved in the soil; when they are swallowed, animals, including rodents, become infected. A person becomes infected with toxoplasma: 1) through the mouth (alimentary, or food way) when eating raw or half-baked meat, minced meat, and more often through objects contaminated with oocysts (from cats); 2) sometimes through the skin of the hands and mucous membranes; 3) in utero (transplacental route).
Clinical picture. Toxoplasma is the causative agent of toxoplasmosis. When a pregnant woman is infected, the pathogen passes through the placenta into the fetus. As a result, the fetus dies (miscarriage, stillbirth) or is born alive with symptoms of acute congenital toxoplasmosis (intoxication, fever, jaundice, damage to the liver, spleen, lymph nodes, nervous system). In a number of cases, outwardly healthy children born subsequently develop mental retardation, visual impairment, etc.
Acquired toxoplasmosis develops when infected after birth. The clinic is varied. The patient's body temperature rises, lymph nodes increase, various internal organs are affected, a rash appears on the skin, etc. Toxoplasmosis can also be asymptomatic.
Diagnostics. Examine blood, cerebrospinal fluid, punctates of lymph nodes, remnants of fetal membranes, placenta, as well as cadaveric or biopsy material. Toxoplasma are found in smears stained according to Romanovsky, histological tissue sections and, in some cases, in a biological test on white mice.
The most accessible intradermal allergic test is stokesoplasmin. Serological methods are also used.
Prevention. To prevent congenital toxoplasmosis, pregnant women are examined with a toxoplasmin test, and if it is positive, serological studies are performed. It is important to follow the rules for keeping cats.
